Contents
What is PCN on Insurance Card?
PCN is a processor control number (PCN) a different identification number that is printed on the health insurance card for health care and it is used to manage the processing of claims for pharmacies to health insurance companies. PCNs can be alphanumeric or numeric. Some companies do not use the PCN.
Check out the below example of Rx Bin, Rx PCN, and Rx Grp:
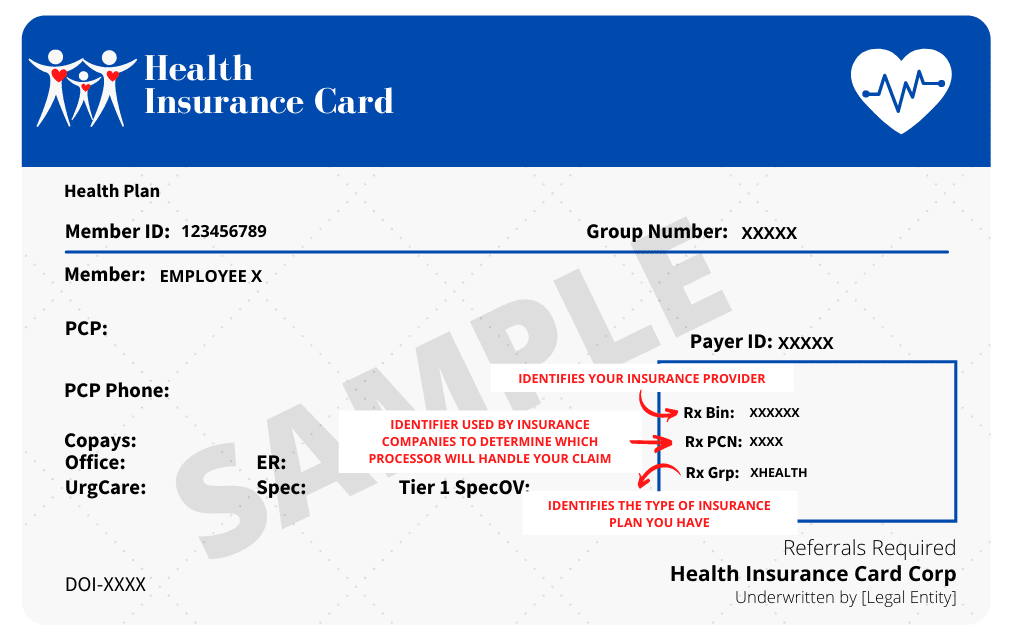
Image Source – houseofdebt
Similar to Rx BIN as well as the Rx Grp code, The PCN is an additional identifier utilized by insurance companies. In the majority of instances, you don’t have to show the PCN of your health insurance every time you visit a doctor’s or pharmacy as they’ll be able to access it directly through the group identification.
However, there are certain scenarios where a doctor or pharmacist may have to enter the PCN manually:
- If you’re covered by private insurance, instead of the employer.
- If you’re seeing someone who’s not part of your network.
- When you use a mail order to the pharmacy.
- Transferring prescriptions between pharmacies.
The doctor could use this information to confirm your eligibility to be covered prior to offering services.
What is RX BIN Number?
The Rx BIN (bank identification number) is the 6-digit number used by health plans to process electronic prescription claims. It is used to inform the pharmacy’s computer database which health insurance company is the one to receive your prescription. During the time that health insurance cards were first issued, the abbreviation “BIN” was created in the banking sector and then changed into the insurance sector. In the end, however, despite their name banks aren’t involved in the process of billing for insurance.
You May Like: PHCS Health Insurance Reviews
What is Rx Grp?
Rx Grp is the group number given by an insurance provider to identify the member’s health insurance plan group. It informs the pharmacy of the type of insurance plan you are on so that they can check the list of approved medications as well as co-pays and deductibles for your insurance plan.
Each plan comes with an individual list of prescribed drugs that are eligible for reimbursement under coverage. If a medicine isn’t listed and found on the list in your plan, it’s not covered.
You’ll require an Rx Grp number at the time of:
- The filling of prescriptions at the pharmacy.
- A new medication you are taking requires prior authorization.
- Be sure to check the prices of medicines prior to visiting the pharmacy.
- Utilizing a pharmacy that mail-orders.
- Sending a reimbursement request to your insurance company.
- The scheduling of a particular medical appointment or procedure.
- To book an emergency room at the hospital.
- Services are being provided by an out-of-network service provider, who must submit a claim on your behalf.
Also Read: Consequences for Getting Sick without Health Insurance?
What to do if you are unable to find your Member ID?
The good news: As mentioned earlier, you are able to access any prescription medication plan without your Member ID card as long as you have the following four numbers which include your Member ID: PCN, Rx BIN, and Rx group.
You can follow the below guide if you don’t have any details of your Member ID Card:
Call your plans Member Services department:
If you can’t locate these numbers, you should call your Medicare program’s Member Services department – to confirm your enrollment and inquire if the new member ID card was issued.
Contact Medicare to get assistance:
If you’re unable to find the policy’s Member Services number, you can call Medicare at 1-800-633-4227, choose the prescription drug option and then select to speak to a Medicare representative. Once you’re connected, contact the Medicare representative to assist you to locate your Medicare plan’s contact details.
Visit a pharmacist:
If you can’t find the Member ID number or a Member ID number, you can bring your Medicare Beneficiary Identifier (MBI) (found on the Red, White blue, and red Medicare card) to your local pharmacy and request the pharmacist to contact the Part D plan to get the Member ID number. Your pharmacist then needs the remaining three numbers needed to fill prescriptions under the Part D prescription drug plan. Your pharmacist might be able to get these by speaking to your Medicare plan.
Difference Between Bins and PCN Code?
All pharmacies utilize BIN or PCN numbers when handling prescription drug claims. The BIN number informs the computer database of the pharmacist whose insurance company is receiving the prescription’s claim. This PCN number is a different identifier utilized to route claims. Three numbers: Rx BIN, Rx Grp, and Rx PCN are the three identification numbers you will find on possibly every insurance card.
These numbers permit your doctor or pharmacy to process claims using the proper channels. These codes identify what kind of insurance you’re under and the type of insurance you’re covered by, and where the claim should be made.
If you do them incorrectly, it could affect the medical coverage you have. For instance, you might be required to pay for your medical bills out of pocket or even denied coverage entirely.
Knowing the meaning of these terms will enable you to maximize your insurance benefits. be a champion for yourself and know the medicines you’re taking.
Posts You May Like:
- The Coverage of Nationwide Pet Insurance Reviews
- Otto Insurance Review – Is it a Scam or Legit?
- PHCS Health Insurance Reviews
- Who Makes Up Medical Information Bureau


